Doctor's Heart Series Chapter 1 : Chronicles of Physician's Heart Attack
Unique perspective from the lens of the Physician as a patient.
Summer of 2021…
It was the beginning of summer, the region was warming up. It was a gorgeous June day and Arjun's 8th birthday. After an incredible daytime adventure and cake cutting, we went to an open-air restaurant on the rolling meadows of Virginia; with breathtaking views, our entire family had a fantastic time. It was indeed vast open fields to run around and with a beautiful setting like the chirping of birds and open skies with beautiful clouds overlying long-distance Washington DC. It was an escape from the day-to-day hustle and bustle, especially since being a physician with my own practice is very hard to take time off. I have enjoyed every moment of it.
Next-Day…
The sudden onset of heartburn started around 5 am. It was not so familiar. I have a history of gastric reflux, but this was a different kind of heartburn. Thinking it was gastric reflux, I popped in a couple of pantoprazole pills, TUMS (antacids). As a physician we jump at taking care of patients, but when its comes to own health, tend to be terrible patients regarding follow-ups, preventive care, and/or seeking medical help. I was uncomfortable with burning pain in the chest, unable to get comfortable, lying down, standing up, or sitting. The pain was relentless and was creeping up, and 10/10 pain ( we usually evaluate patients for the pain score 1 is the no pain and 10 is the most pain). This symptom was ongoing for more than an hour. My wife Radha ( physician herself), worried about seeing what's going on with my symptoms, advised our drive to the ER(Emergency room) for further evaluation (married men tend to be live longer than single men, this must be one of the reasons). I reluctantly agreed as the pain was not getting any better. As she drove to the ER, I initially thought of going to the closest satellite ER. However, Radha suggested we go to the main hospital ER ( which was the right decision we will find out later).
In the Hospital ER…
The most familiar place I have ever been after my home. I worked in this hospital for more than 8 years and have been to the ER hundreds of times to admit and treat patients. As I stepped into to ER, this time as a patient, flashing lights and hallways didn't appear to be the same(every second felt like an hour, and I remember every tiny detail as I wheeled down). There was an eerie feeling as I was wheelchaired from the registration. As they were placing me on the bed, flashes of previous patients in that room came flashing; it was bed #21. Throughout my career, many patients with chest pain; we evaluate them for life-threatening conditions (common ones to rule out are Heart Attack, Blood clot in the lungs, tear in the inner layer of the aorta called dissection, rupture of the esophagus, collapsed lung, Pneumothorax). A million diagnoses were going in my mind. I was confident about possible Dissection of the Aorta. On the bed, they started hooking me to the monitors, asking me questions about what was going on and what were my symptoms. I was greeted by my Colleague(surprised to see me as a patient), who was my attending doctor during the shift. I was in a lot of pain; as they were doing my EKG(Electrocardiogram), I saw my own EKG showing a significantly abnormal EKG with ST-elevation( Heart attack). My heart sank. I felt my whole world come crashing on me, a lot of roller-coaster emotions. Code was called( Emergency on-call alarm, indicating a significant event happening in my room). Everyone came rushing to the room. I was lying there emotionally as Radha watched me helpless in this condition. Cath lab team arrived. In medical lingo, there is something called door to balloon time. Once a Heart attack is diagnosed (heart attack diagnosis to coronary angiogram should be less than 90 min), Studies have shown that the door to balloon time actually improved significant outcomes in recent years. While preparing for Cath lab, I was given aspirin (anti platelet (shown to reduce mortality), nitroglycerin (which helps to dilate the heart vessels so better circulation to the heart and eases pain), morphine (which helps with relaxation and pain). Nothing was alleviating the pain; I have received multiple doses of morphine; still the pain was at this time was 20/10 in intensity.
Cath lab team arrived…
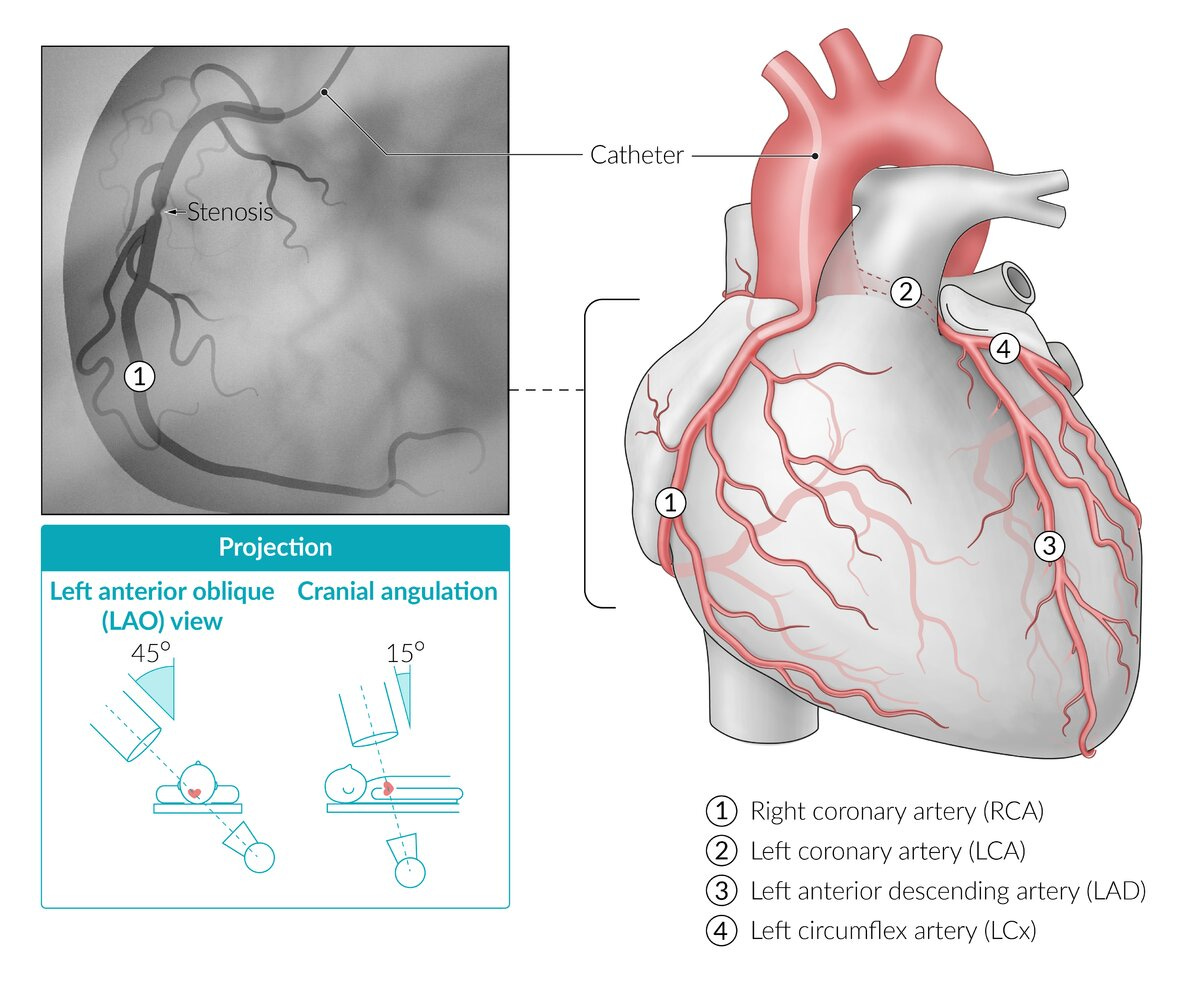
In the Cath lab (Heart Catherization procedure room), I was lucky to have one of the best Interventional Cardiologists on Call. I underwent an emergent Coronary Angiogram with Angioplasty (Angiogram is the procedure guide-wire being placed through the arteries in the groin or wrist using the small amount of iodine contrast look at the coronary arteries under the guidance of fluoroscopy). My right wrist was used to undergo an angiogram (I have sent many of my patients to undergo a coronary angiogram before, and now the life saving procedure, to think about it was insane). I was given small doses of anti-anxiety medication to have the minimal effect of the procedure. During the angiogram procedure, I was noted to have complete occlusion of the right coronary artery with the ruptured plaque (plaque is buildup of fatty deposits in arteries). People with coronary artery plaque amount 30 % - 40 % can rupture causing complete occlusion resulting in heart attack and sudden death as reported in the previous autopsies. The mortality goes as high as 30% in this category with a first-time heart attack. Surprisingly this is way too common in the Asian Subcontinent, where I grew up before immigrating to the US. Heart disease is still the number one killer in the United States, carries significant morbidity and mortality.
During the procedure of right-sided angioplasty with placement of stent, small clot moved distally, causing irritation to the heart, soon after developed Abnormal heart rhythm called Ventricular fibrillation (A life-threatening heart rhythm that results in a rapid, inadequate heartbeat), requiring a total of 6 shocks to bring back to a normal regular rhythm. As the anxiolytic waning off, I vaguely remember the last shock even to this day gives me goosebumps, I vividly remember jumping off the bed, floating in the air, like in the matrix movie. I was later moved to the ICU for closer monitoring.
Intensive Care Unit…
During the first 24 hrs, the chance of recurrent arrhythmias (abnormal rhythm to the heart) is the highest; hence it was closely monitored in the Medical ICU. My Troponin level (Cardiac biomarker, refers to heart muscle injury, higher the worse) was severely elevated by this time; it was more than 32, (normal<0.04). I also underwent Echocardiogram to assess the right heart, showed right heart weakness. The shocks really made me extremely weak and fatigued. I round with ICU nurses regularly; this was the first time I have witnessed the direct patient (me) care from these lovely nurses, who were absolutely fantastic. The use of urinal in bed, the blood draws, constant beeps, uncomfortable bed, etc., had an experience. In fact, my patient, who I was treating and managing the previous day, was still there next door as I was enquiring with my nurse(Doc, please take care of self, patients ain’t going anywhere). The pain slowly subsided; however, the electrical jolt was causing extreme fatigue. The familiar ICU, which I usually round to see my patients, is suddenly on the receiving end. Until this time, I have been very healthy. (so I thought, Atherosclerosis, plaque in the arteries takes years to build, some can be familial or genetic preponderance and some lifestyle, combination of both, lately looking at data shows that being south Asian descent itself is the higher risk). The only history I had until this time was Gastroesophageal reflux disease. While I was trying hard to manage and treat my patients, it was my turn to be saved.
Background…
I am 43 year old Internal Medicine Physician, BMI 25, Physician of Indian origin, finished my residency in Chicago. Started working in New Jersey post-residency as Hospital Medicine Physician for 5 years, later moved to Northern Virginia outside Washington DC, been there since. I started my solo practice 3 years ago, after working in the hospital setting as a hospitalist for almost a decade ( treating acute illnesses in the hospital). Due to its monotonous nature, I quit the well-paying job. I started Internal Medicine ( Doctor specializes in acute and chronic diseases of adults ) practice with the only intention of helping patients giving them an abundance of time, concentrate more of preventing patients going to the hospital. In US, there is paradigm shift in relation to the patient care, as the care drifting away from solo practitioners to big groups controlled by corporations, the doctors are burnt out due to the imposing pressure to generate more rvu's(reimbursement), increasing paperwork and the unending clicks of electronic health records. Initially, I hustled like any other business getting patients; I used to work in the hospital, take calls, cover other doctors' patients, and care for long-term care patients. Soon the practice was growing; I was working 24/7 and had ongoing physical exhaustion (sleep deprivation, poor eating habits, less exercise, undue stress from above etc.).
“The practice of medicine has been overtaken by the alarm bells of technology”.
Causes…
As the news spread, questions started arising regarding my heart attack. Everyone(my friends and colleagues) has been stumped due to the sudden nature of my heart event. At this time, we were all pondering the causation for my acute event. The patients with Atherosclerosis of heart (Plaque build-up of fats, cholesterol, and other substances in the artery walls), science is at infancy why certain population are more prone for plaque rupture causing heart attack than others. I am an avid runner; I run a couple of times a week. I had successfully completed a half marathon the prior year. I had a slightly abnormal cholesterol. There are models, to determine use of statins(cholesterol lowering medications) for prevention. Most of the models has been done and validated mostly for Caucasians and less likely Asian counterparts, my risk was literally so low to take medications.
There are a few things I probably might have exaggerated; since I started my own practice 3 years ago, the most significant sacrifice I had made was sleep deprivation due to being on call every single day. The number of calls has gone up, and technology and medicine have been intertwined more than ever. The time for exercise suffered in the last few months prior to event. Stress from running day to day operations business side of it and compassion fatigue (emotional stress caring sick patients). The diet poor in nutriton due to lack of time.
Solution…
Since last 6 months, I have been questioning myself and looking into heart disease and prevention. Mediterranean diet has helped significantly to reduce heart disease(rich in greens, olives, nuts, wine etc, less carbs). Raw vegetarian, I call them live foods (eating more raw vegetables/greens, fruits and unsalted nuts, more the better), limit alcohol and meat. Exercise is a must, 30 min a day (just brisk walk 15 min in one direction and return). It is essential to get sleep for 6-7 hrs per day. Limit screen less than 2 hrs a day(what am I talking?) and avoid prolonged sitting. Blood pressure is the corner stone of healthy heart, keep the blood pressure optimized. Checking Lab work especially attention to lipid profile yearly (Non HDL needs to be within normal limit), fasting blood sugars, HBA1c and glucose tolerance test(early diagnosis of Insulin resistance or pre diabetes). In my opinion, BMI(scale shows if one is obese or not) doesn’t fit the criteria for South Asians, but waist line does (men over 36 inches and women over 32) tend to have high insulin resistance and can carry disease, work towards trimming your waistline. Mindfulness does help to focus (when mind is free of clutter so does the body). Everyone is different and follow with your doctor to optimize and prevent chronic diseases.
Conclusion…
I was discharged from the hospital. The idea of doom had an impact with wildly running of emotions. The familiar place where I was doing medical rounds until 2 days ago, now I was the patient. Currently, my interest in studying the affect of heart disease on south Asians. According to World Health Organization, 30 % of global fatalities happen secondary to Heart disease; 60 % of heart disease comes from the Asian subcontinent. The need for more significant research and education to combat heart diseases in the South Asian population.
Six months after…
I am currently on maximum medical therapy to prevent recurrence, I underwent repeat ultrasound of the heart(back to normal function). I significantly cut down alcohol and meat. I am trying to become raw Vegetarian(less cooked and processed foods). I have made significant changes at work, I have stopped going to hospital, calls have been tremendously reduced. Enjoying better quality sleep. I am trying to do more quality work in prevention of disease among my patients and community.
Suman Manchireddy MD FHM FACP Internal Medicine







So relieved that you are back to normal. I loved the post because it made my feet curl. My body stiffened as I read through the ordeal you went through.
The tiny humorous bits (ex - what am I talking?) are well, tiny and they didn’t soften the message that you have taken great pains to put together for us. The assessment (20/10) bit expressed exactly what you wanted to express.
If I could make a request, I would really love it if you could double click on ‘tech alarm bells’ part. There is way too much medtech and I know of people who are fit, eat well, sleep well but are still sad because their BMI machine is telling them that they are laterally obese. The part about medicine/diagnosis assessment being ignorant about asian body type could also be extrapolated. Look at me making silly demands!
I am so glad you have started writing here. Do tell us sometime why spyderdoc?
Sanskaari cheers with orange juice, Suman!
An innocent narration of event experienced by doctor self .... Helpful to understand and carries few take aways.