Earlier in my career, I started as a nocturnist (night doctor) working in a tertiary care hospital; being a recent grad physician, I was enthusiastic about working and learning simultaneously as this tertiary care hospital with 800 beds and only a few providers at night. One night, code blue ( code blue is called when a patient is in serious trouble, either not responding or unconscious) was called around midnight. We pace to where the code blue was called where we noticed patient heart rhythm was in asystole(heart stops beating). Upon arrival, I noticed he was all tubed, and CPR or cardio pulmonary resuscitation( rapid pressing of the chest to revive the patient when they are pulseless and not breathing) was already started; the room atmosphere was intense, and things were beeping in behind. As I enquired about the case, he is an elderly gentleman in his late 80s who was admitted to the ICU for respiratory failure(lung failure) and was intubated. He had many chronic ailments and was on various medications, antibiotics, pressors(medicines to support blood pressure), and IV fluids. Despite 20 minutes of efforts to restore the pulse, including administering all emergency medications to improve heart rhythm, we were unable to revive the patient. The patient passed away from respiratory failure secondary to influenza infection. Though this is rare, it does happen, especially in the vulnerable population.
Many of my colleagues fight these microscopic adversaries in the ICU from time to time, with some emerging victorious and others facing defeats.
In the Early 20th century, we were hit with one of the world’s worst pandemics; the Spanish flu(H1N1)pandemic killed nearly 20 million around the globe. Later, more minor influenza pandemics and the recent COVID-19 pandemic(a once-in-a-century pandemic) wreaked havoc on human life. Yet the world is vulnerable to the next pandemic, perhaps even more than in 2019 when the pace and frequency of global travel were considerably higher every year. We are learning from the old pandemics and leaving clues for the next pandemic as we have yet to determine where it will come from. In the US, the CDC estimates an average of 30000-36000 flu-related deaths per year over the past decade, depending on the severity of the flu season. These figures primarily reflect deaths from respiratory illnesses directly caused by the flu. However, influenza can also lead to complications such as heart attacks or bacterial pneumonia, which can significantly increase the overall death toll.
I realize we take the flu for granted; Does the vaccine work? Does it really make a difference if we take it? Let’s delve into the details.
What is Flu ?
Flu is a contagious respiratory illness caused by influenza viruses that infect the nose, throat, and sometimes the lungs.
What is the Influenza Virus?
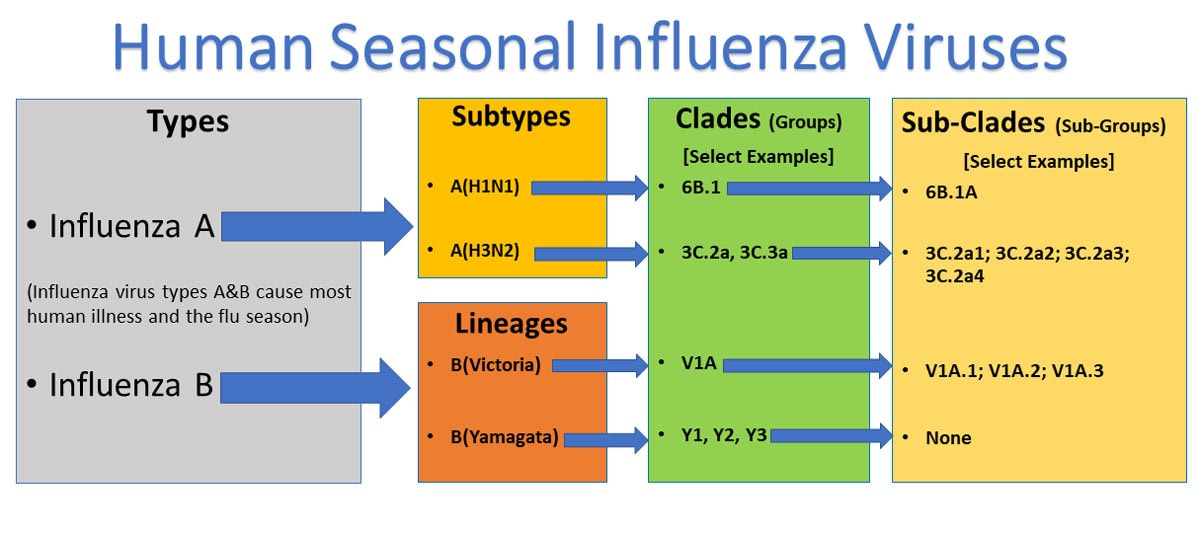
Influenza Viruses are a family of Orthomyxoviridae. They are a type of enveloped viruses with a genome consisting of negative sense-stranded RNA, including 4 genera or viruses: A, B, C, and D. Influenza A and B are the leading cause of annual flu outbreaks in humans, with influenza A further classified into subtypes based on their surface glycoproteins hemagglutinin (HA) and neuraminidase (NA). 18 HA subtypes (H1 H18) and 11 NA subtypes (N1 N11) are currently known; most notable today are the H1N1 and H3N2 subtypes that co-circulate in the human population. Since the 1970s, influenza B has diverged into two lineages based on antigenicity, the Yamagata and Victoria lineages. It's important to note that C & D rarely cause infections in humans, providing some reassurance about the low risk of these viruses.
Antigenic drift refers to the gradual accumulation of point mutations(changes in the genetic material) in the influenza virus’s surface proteins, HA and NA, allowing the virus to evade the host immune system and create new strains. Antigenic shift, on the other hand, involves the reassortment of gene segments between different strains, leading to major changes in the virus's structure and often resulting in pandemics, such as the 2009 H1N1 outbreak. Due to these constant changes, seasonal influenza vaccines must be updated annually. The World Health Organization (WHO) coordinates this process through its Global Influenza Surveillance and Response System (GISRS), which monitors global virus trends and issues vaccine recommendations for each flu season.
History of Flu Vaccine…
After the Spanish flu in 1918, it was the work of a few scientists before World War 2. Who has isolated the strains of influenza virus? The history of the flu vaccine dates back to the early 20th century when researchers began to understand the influenza virus and develop ways to prevent its spread.
In 1933, British scientists Wilson Smith, Christopher Andrewes, and Patrick Laidlaw isolated the influenza A virus, marking a breakthrough in understanding the cause of flu.
Influenza B was discovered in 1940. In 1942, during World War II, the U.S. Army collaborated with microbiologist Thomas Francis Jr. and Jonas Salk (who later developed the polio vaccine) to develop the first inactivated flu vaccine.
The first approved flu vaccine was distributed to the public in 1945 in the U.S., targeting the influenza A virus.
By 1947, a bivalent vaccine that could protect against influenza A and B was developed. This two-strain approach became the foundation for future vaccines. Flu vaccines became widely available for civilian use in the 1950s.
In 1978, trivalent vaccines, which included two influenza A strains and one influenza B strain, became standard.
In 2012, the first quadrivalent flu vaccine was introduced. This vaccine added a second influenza B strain, offering broader protection.
What is a Vaccine ?
A vaccine is a laboratory preparation of a specimen of a particular antigen(foreign substance, protein from virus, bacteria, etc.) that provides immunity to a specific disease. It stimulates the body’s immune system to recognize and fight particular pathogens.
Introduction of Antigens—> Immune response activation—>Memory Formation —>Protection
After the introduction of antigens, either through injection form or through the nasal route, the body goes through changes to that particular antigen and starts to work to activate the immune system, that is, the lymphatic system. As the body recognizes a foreign body, it starts producing antibodies by activating specific immune cells to fight and neutralize the foreign body. The immune system also creates the memory cell to remember the antigen or the foreign for future exposure(I can’t believe we have so many systems working without thinking twice; imagine if they worked for money or other perks, we would have been dead a long time ago…lol). Because of this immune memory, the body can quickly and efficiently respond to the pathogen, preventing illness or reducing its severity. Essentially, vaccines are a powerful tool in our arsenal, preparing the immune system to combat specific infections without causing the disease itself. This preventive measure is a reassuring safeguard for our health.
There are different ways vaccines are produced. The most common method for flu vaccine production involves injecting the selected virus strains into fertilized chicken eggs. The viruses are allowed to replicate, and then they are harvested, inactivated, and purified for use in the vaccine. This method has been used for over 70 years. A newer method, cell-based flu vaccines, uses animal cells (instead of eggs) to grow the virus and the third method does not require the flu virus at all. Instead, scientists isolate a gene from the virus and use it to create proteins that trigger an immune response. There are different ways to obtain the vaccine but the idea is to protect against the virus.
Multiple studies have confirmed the protective effects of the flu vaccine, although its effectiveness can vary depending on the match between the vaccine strains and the circulating viruses. Here are the key findings:
Flu vaccines reduce the risk of illness by 40% to 60%.
Protection of the vulnerable population Children, Pregnant, and Elderly ( cuts down death by 30 to 60%)
Herd Immunity: While the flu vaccine protects individuals, it also contributes to herd immunity. By reducing the overall number of flu infections in a community, vaccinated individuals help protect those who cannot receive the vaccine.
Real-World Studies: Every year, real-world studies are conducted to assess the effectiveness of the flu vaccine during a particular season.
High Dose vaccines, especially for vulnerable populations, to better fight infections and increase the immune response.
Universal Flu Vaccine(Can’t wait!): Researchers are developing a universal flu vaccine that would provide long-lasting protection against multiple flu strains, potentially eliminating the need for annual vaccinations.
Each year, the flu vaccine is formulated to protect against the most common and likely circulating strains of the influenza virus, as the flu virus evolves constantly. Typically, the vaccine targets strains from two main types of influenza viruses: Influenza A and Influenza B, which are prevalent during most flu seasons. There are two primary types of flu vaccines available. The trivalent vaccine protects against three strains: one Influenza A H1N1 strain, one Influenza A H3N2 strain, and one Influenza B strain (from either the Victoria or Yamagata lineage). The quadrivalent vaccine offers broader coverage, protecting against four strains: one Influenza A H1N1 strain, one Influenza A H3N2 strain, and two Influenza B strains (both Victoria and Yamagata lineages).
More than a decade and a half has passed since that night, yet I remember it as if it were yesterday. The patient I encountered in the ICU later discovered he was not vaccinated. Sometimes, I wonder if this small virus can do so much damage(Yes! Remember Spanish flu). As a new graduate, I remember vividly that day I encountered the deadly flu for the first time. Since then, I have treated and cared for many patients with the flu and some severely ill patients in the ICU. Flu is a terrible feeling that can cause mostly mild symptoms like fever, headaches, nasal congestion, malaise, muscle aches, and rarely severe symptoms. I hope everyone reading here gets the Flu vaccine unless you have specific reasons. With over 70 years of successful use, the flu vaccine is a reliable and effective way to protect yourself and your loved ones. It's a safe choice. So talk to your doctor and go ahead and take your jab today(available from September 2024).
Let’s do a quick Q&A session!
Does my doctor get a flu shot?
Yes! Most medical staff are vaccinated for influenza (especially in our office). This reduces symptoms and prevents the virus from spreading to others, especially to the vulnerable.
How does the Flu spread?
People with Flu can spread it to others. Flu viruses spread mainly by droplets made when people with flu cough, sneeze, or talk. So, if you are sick, cover your cough and mask it.
I have an egg allergy; what should I do?
Yes, most people with egg allergies can safely receive the influenza vaccine. Still, the approach depends on the severity of the allergy and the type of vaccine: Most flu vaccines contain only trace amounts of egg protein. These vaccines are safe for most people with egg allergies, including those with a history of severe egg allergy. For those with severe egg allergies or a history of anaphylaxis, egg-free flu vaccine options, such as the recombinant influenza vaccine (Flublok), which contains no egg proteins, are available. Talk to your physician.
I am a healthy adult; do I really need one?
CDC thinks yes! It recommends anyone above 6 months of age get a yearly influenza shot. It reduces the risk of illness, prevents severe outcomes, reduces spread, provides herd immunity, and can be mild. In summary, even for healthy adults, the flu vaccine offers essential protection for yourself and the broader community.
What kind of side effects do I get from taking an Influenza Vaccine …
Most reactions to vaccines are mild and temporary, such as soreness at the injection site, mild fever, or fatigue. Serious adverse events are rare and can occur in sporadic instances. However, these are usually not directly caused by the vaccine but could be related to underlying health conditions or coincidental events. The risk of serious harm from the vaccine is far outweighed by the risk of severe illness or death from influenza.
Why is Flu only in Western countries and not here in tropical countries like India :
Flu is present all over the globe, with different strains of influenza affecting humans. Interestingly, places like India or other tropical countries are so prominent that multiple viruses compete to create a significant infectious disease burden. Most tropical countries already deal with various infectious diseases, including malaria, dengue, typhoid, hepatitis and chikungunya. Influenza is the least on their minds.
What is the Annual Efficacy of the vaccine?
The flu vaccine’s effectiveness typically ranges from 40% to 60%. This variability is due to factors such as how well the vaccine strains match the circulating virus strains in a year.
What is the chance that a vaccine is received for one strain and then encounters a different strain? What happens?
The protection provided by a flu vaccine primarily depends on how well the strains included in the vaccine match the circulating strains of the influenza virus. If the strain you encounter significantly differs from the vaccine strain, the vaccine may offer limited protection. Influenza vaccines stimulate the immune system to recognize and fight influenza viruses.
Where can I get it?
From September to February, the flu vaccine can be obtained at any pharmacy or doctor’s office in the US. Most insurances cover it, making it easily accessible for everyone.
How long does it take to get complete antibody protection from the vaccine, and what is the best time to take it?
14 days / September - October every year.
Since we are on the topic of the Flu, how do we treat it if we get Flu?
Oseltamivir or Tamiflu is effective against the Flu. It reduces the severity and the number of days of sickness. But prevention is always better than cure, so get your jab if you want a milder winter.
Suman Manchireddy MD FACP FHM, Internal Medicine, Leesburg, VA.
Email : Care@ReliantMD.com
Disclaimer: This is purely informational and educational purposes only, seek medical advise prior to starting any testing or treatment regimen. The data presented here is researched extensively and has been condensed for a broader audience.
References…
1. The 2010-2011 Seasonal Influenza Vaccine Effectiveness Study (McLean et al., 2012
2. The 2018-2019 Study on Influenza Vaccine Effectiveness (Flu VE Network, 2020).
The Cochrane Review on Influenza Vaccines (Jefferson et al., 2018)
https://jbiomedsci.biomedcentral.com/articles/10.1186/s12929-020-0626-6
who.int/en/news-room/fact-sheets/detail/influenza-(seasonal).
https://archive.cdc.gov/www_cdc_gov/flu/pandemic-resources/1918-pandemic-h1n1.html
CDC