36. Suzetrigine: The FDA Recently Approved a Breakthrough Non-Opiate Medicine for Acute Aain Management.
A promising alternative in the struggle against opioid dependence.
Last night, again on TV for the nth time, the anchor mentioned that more than a hundred thousand people will die from opioid overdoses in the USA(unbelievable!). As a medical professional working hard to save lives, I find it disheartening that preventable causes are leading to death and despair. There should be a zero-tolerance policy regarding opiates, especially drugs that make their way into the USA. These drugs are mostly synthetic, manufactured in remote labs or facilities, and are 50 to 100 times more potent than ever. Despite our progress in protecting citizens from the opioid epidemic, the CDC notes that more than 70% of the drugs involved are synthetic fentanyl. So, let's examine the actual physiology of how these medications work and the ongoing discussion around non-opioid medications for acute pain. Finally, after more than 20 years, new forms of medication are emerging that bypass the pleasurable effects of traditional opioids, which cause central nervous system effects that lead to addiction and other side effects.
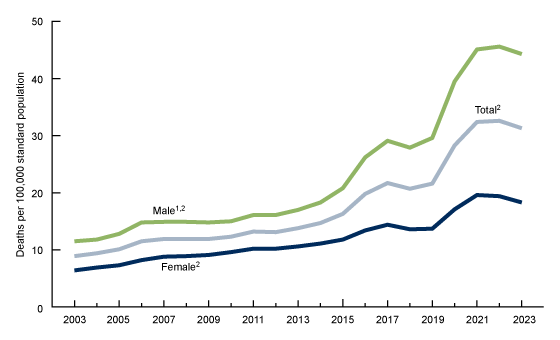
In the last two decades, the mortality rate due to drug overdose in the United States has exhibited significant fluctuations. The age-adjusted overdose death rate escalated from 8.9 per 100,000 in 2003 to 32.6 in 2022, subsequently experiencing a slight decrease to 31.3 in 2023, with a total of 105,007 fatalities recorded in that year. This increase was predominantly attributed to opioids, especially synthetic opioids such as fentanyl, which accounted for approximately 73,654 deaths in 2022—over twice the figure reported in 2019.
As humans, pain is inherent to us. There is no person in this world who has not experienced pain in some way. That's nature. Most of the time, it is transient, and we learn to cope with it and manage it better. In some cultures, pain is something people live with; there are no medications or drugs available to help, so they either endure it or use alternative modalities. However, in more advanced societies, pain tolerance tends to be lower, possibly because the amount of hardships faced is much less, which may significantly affect pain perception. Let’s explore pain and its modalities and also discuss the new drug that is revolutionizing the treatment of pain.
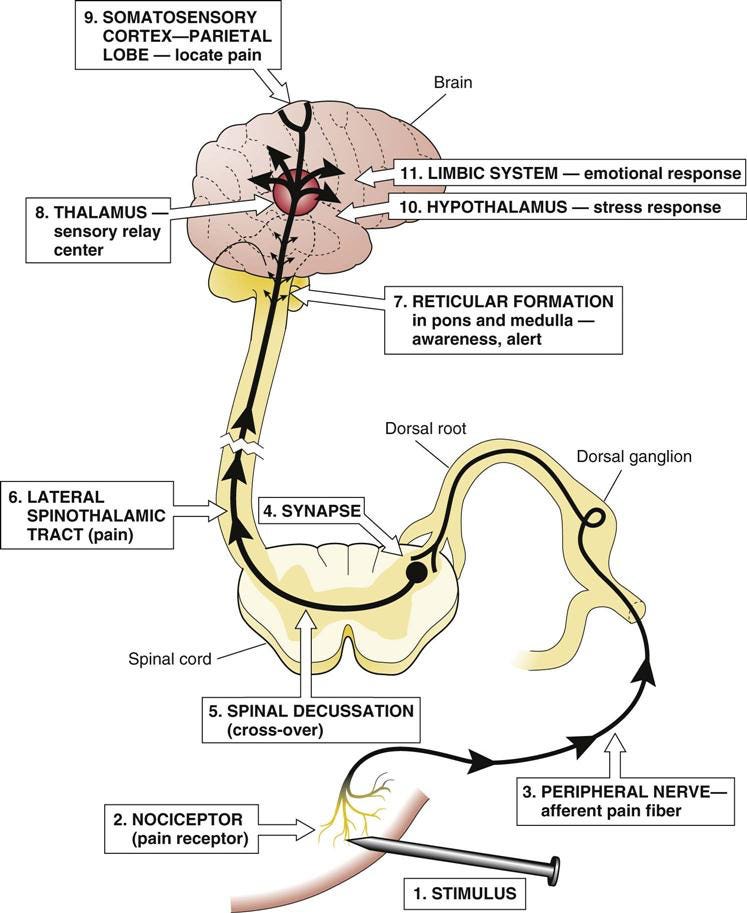
What happens to pain when we experience a minor cut or when something affects the skin or other structures? The human nervous system is highly evolved and consists of various parts, such as the brain, the spinal cord, and peripheral nerves, as shown in the figure below. When pain is felt on the skin due to a cut or bruise, the nerves around the affected area become activated and send signals to the brain, triggering various chemical reactions throughout different areas of the nervous system, from the local area to the brain. In response to this activation, we react to external stimuli, whether from a thorn or a burn, instinctively trying to move away from the source of the stimuli.
The pain pathway is interesting as it involves four distinct steps: transduction, transmission, modulation, and perception. Pain begins when nociceptors (specialized sensory receptors) detect harmful stimuli, such as extreme temperature, pressure, or chemical changes, triggering electrical signals (transduction). These signals travel through A (fast) and C fibers(slow). The spinal cord relays the signal to the brainstem and then to higher brain centers like the thalamus, somatosensory cortex, limbic system, and prefrontal cortex, where the pain is interpreted (perception).
Ethnic Variability in Pain Perception: A Clinical Study explored differences in pain perception across ethnic groups, revealing significant variations in self-reported pain scores and physiological responses. East Asian participants reported the lowest pain perception, while those of African descent exhibited the highest, showing increased pain scores and stronger physiological responses. Caucasian individuals had moderate pain perception, with scores falling between the two other groups. These differences were influenced by genetic, cultural, and psychological factors, highlighting the complexity of pain tolerance and reporting across diverse groups.
The brain then attempts to regulate pain through descending regulatory pathways, releasing excess neurotransmitters that inhibit, such as endorphins, serotonin, and norepinephrine, to help decrease the pain signals. Thus, the system ensures that pain is processed, perceived, and regulated appropriately, influencing our response to injury or illness. These pathways from the midbrain to the brainstem release Endorphins and Enkephalins, natural opioids that block pain signals. Serotonin and norepinephrine inhibit pain transmission in the spinal cord. GABA and glycine act as neurotransmitters that inhibit and dampen pain signals.
Per Melzack and Wall's suggested theory, non-painful stimuli can "close the gate" in the spinal cord, preventing pain signals from reaching the brain. Utilizing local measures like cold therapies, lidocaine, and other local methods activates non-painful A fibers, which block pain signals from transmitting to the brain.
There are currently many pain modulation therapies. These therapies alter how pain signals are transmitted, perceived, or inhibited. They can be pharmacological (medications) or non-pharmacological (lifestyle and interventional techniques) and target the descending inhibitory system, neurotransmitters, and spinal cord mechanisms to effectively control pain.
Pharmacological therapies for pain management involve various classes of medications, each targeting specific mechanisms to reduce pain. Opioid analgesics such as morphine, oxycodone, and fentanyl mimic endorphins and bind to mu-opioid receptors in the brain and spinal cord, effectively blocking pain signals and used for severe pain like post-surgical or cancer pain. Antidepressants, including duloxetine (Cymbalta), amitriptyline, and venlafaxine, increase serotonin and norepinephrine in the descending pain modulation pathway, helping to manage neuropathic pain, fibromyalgia, and chronic back pain. Anticonvulsants like gabapentin and pregabalin stabilize nerves by blocking calcium channels, offering relief for conditions like diabetic neuropathy and fibromyalgia. NMDA receptor antagonists, such as ketamine and dextromethorphan, prevent central sensitization and chronic pain by blocking NMDA receptors, making them practical for complex regional pain syndrome (CRPS) and severe chronic pain. Finally, anti-inflammatory medications like NSAIDs (ibuprofen, naproxen) and corticosteroids (prednisone, dexamethasone) reduce inflammation, alleviating pain associated with autoimmune or chronic inflammatory conditions.
Non-pharmacological therapies provide effective pain management by targeting the body’s natural pain modulation systems. Transcutaneous Electrical Nerve Stimulation (TENS) uses mild electrical currents to stimulate A-beta fibers, blocking pain transmission. It is commonly used for neuropathic pain, arthritis, and postoperative pain. Acupuncture stimulates the release of endorphins and activates descending inhibition, offering relief for chronic pain, migraines, and osteoarthritis. Cognitive-behavioral therapy (CBT) helps reframe pain perception and reduce stress, activating dopamine-mediated pain inhibition and is effective for chronic pain, fibromyalgia, and psychosomatic pain. Physical therapy and exercise strengthen muscles, improve circulation, reduce inflammation, and activate endogenous pain modulators, making them beneficial for back pain, joint pain, and post-surgical recovery. Mind-body therapies, including meditation, yoga, and biofeedback, enhance relaxation, reduce pain perception, and lower stress-related inflammation, helping to manage fibromyalgia, chronic migraines, and tension headaches. Lastly, spinal cord stimulation (SCS) involves implanted electrodes that disrupt pain signals before they reach the brain, providing relief for failed back surgery syndrome and
Using minimally invasive techniques, Interventional procedures provide targeted solutions for severe, refractory pain. Epidural steroid injections (ESI) help reduce inflammation around nerve roots, relieving conditions such as sciatica and herniated discs. Nerve blocks involve injecting anesthetics around specific nerves to alleviate pain from migraines or chronic regional pain. Radiofrequency ablation (RFA) utilizes heat to destroy nerve endings, effectively interrupting pain signals and providing long-term relief for arthritis and spinal pain. These procedures can significantly enhance the quality of life.
Opioids…
Let's get into the details in regards to opiates, as these are the major contenders in morbidity and mortality, and understand what's happening in the neurochemicals to better understand why we are so addicted to these chemicals. Opioids operate by binding to opioid receptors (mu, kappa, and delta) located in the brain, spinal cord, and other areas of the body. This process blocks pain signals and induces feelings of euphoria and relaxation. When opioids activate these receptors, they inhibit the release of neurotransmitters like substance P and glutamate, which play a role in pain transmission. Simultaneously, they enhance dopamine release in the brain’s reward system (ventral tegmental area and nucleus accumbens), reinforcing pleasure and potentially leading to addiction.
When opioids activate these receptors, they inhibit the release of neurotransmitters like substance P and glutamate, which play a role in pain transmission. Simultaneously, they enhance dopamine release in the brain’s reward system (ventral tegmental area and nucleus accumbens), reinforcing pleasure and potentially leading to addiction. Opioids are highly addictive due to their impact on the brain's reward system, which floods the brain with dopamine, creating intense pleasure and reinforcing drug-seeking behavior.
Opioids are highly addictive substances that impact the brain’s reward system, whenever the opioid medication is taken the brain is flooded with the dopamine hence creating the intense pleasure and euphoria and relaxation. Thus these medications increasing the drug seeking behaviour. Hence the Opioids need to be last resort for managing pain, if needed may consider few pills for severely acute pain.
Over time, the brain builds tolerance, requiring higher doses for the same effect, and withdrawal symptoms, including flu-like symptoms, body aches, nausea, and intense cravings, make quitting difficult. This leads to psychological dependence, with emotional numbing and a trigger-response cycle that further fuels addiction. Potent and fast-acting opioids like fentanyl and heroin are especially addictive, and social and environmental factors, such as overprescription and easy access, increase the risk. Despite the challenges, medications like Methadone, Buprenorphine (Suboxone), and Naltrexone can help manage cravings and withdrawal, making opioid addiction a complex condition to treat but not impossible to overcome.
Even taking a few pills can lead to dependence on the drugs. With hundreds of thousands of people dying every year, we must explore better options. We need to reserve our dopamine for better use. Obviously, technology is taking over; that's another topic endless dopamine flowing no end in sight(that will be next topic of discussion, LOL), but we have examined non-opioid alternatives, what we have, and what is in the pipeline, and that excites me. Here is the new generation of non-opioid medications that have been clinically approved by the FDA. Leading a path to avoid unnecessary deaths.
In a Clinical study published in the BMJ, comparing the effects of NSAIDS or NSAIDS with Acetaminophen vs Morphine in acute pain in closed fractures. The study findings suggest that ibuprofen and its combination with acetaminophen have similar or better analgesic effects compared to morphine in patients with closed extremity fractures. Although morphine initially provided the greatest pain relief, its effect diminished over time. In contrast, ibuprofen and the ibuprofen-acetaminophen combination maintained their analgesic effects for a longer duration. The combination therapy demonstrated the most sustained pain reduction. The study highlights the potential of non-opioid analgesics in fracture pain management and emphasizes the importance of initiation of these medications as first line analgesic for patients with fractures. These findings support the growing trend of exploring non-opioid analgesics in pain management.
Suzetrigine or Journavx :
The Food and Drug Administration recently approved a new non-opioid medication called Suzetrigine, which is currently sold under the brand name Journavx. This drug is effective in treating moderate to severe acute pain in adults. It targets the peripheral nervous system rather than the central nervous system, thereby reducing the central side effects commonly associated with treatments, particularly opioids, and eliminating the risk of addiction and even sudden overdose and death.
To review the action mechanism, refer to the previous diagram featuring the Dorsal nucleus within the peripheral nervous system. When an injury occurs, like stepping on a nail, pain-sensing nerve cells in the affected area trigger nerve impulses to signal the brain, similar to Morse code. These signals arise from nerve impulses generated by molecules known as sodium channels. Like gates, sodium channels open to permit charged sodium ions to enter the nerve cells. The electrical currents produced by these sodium channels generate nerve impulses that transmit pain signals to the brain. Sodium channel blockers inhibit the function of these channels, thereby reducing the nerves' ability to effectively transmit pain messages to the brain.
The sodium channel NaV1.8 is selectively expressed in peripheral neurons, including the neurons of the dorsal root ganglia that transmit nociceptive signals. Suzetrigine is an oral, small molecule that potently inhibits NaV1.8 currents and shows a higher selectivity for NaV1.8. No other expression was noted in the central nervous system, so the drug has minimal effects on the brain.
Most common pain conditions originate in the periphery, where dorsal root ganglion and trigeminal ganglion neurons transmit pain information to the CNS. Voltage-gated sodium (NaV) channels drive neuronal excitability, and three subtypes - NaV1.7, NaV1.8, and NaV1.9 - are preferentially expressed in the peripheral nervous system, suggesting that their inhibition may treat pain while avoiding central and cardiac adverse effects. Genetic and functional studies of human pain disorders have identified NaV1.7, NaV1.8, and NaV1.9 as mediators of pain and validate
Novocaine, a local anesthetic widely used in dental offices, is a sodium channel blocker but not selective. This means it doesn’t target a particular sodium channel; instead, it numbs the area where it is applied. Suzetrigine, however, acts within the peripheral nervous system to block Nav1.8, which Dr. Waxman’s team showed is responsible for sending pain signals to the brain. The medication reduces the pain signals before they can reach the brain.
The trial was published in the NEJM, and Suzetrigine was tested in each of about 1,000 patients who experienced moderate-to-severe pain after surgery. Participants were divided into three groups: One received a placebo, one got the opioid Hydrocodone, and the third was Suzetrigine.
Both trials, one involving abdominoplasty patients and the other bunionectomy patients, demonstrated the impressive effectiveness of suzetrigine. The study showed that it could ease pain as effectively as Hydrocodone, a well-known opioid, and both medications provided more pain relief than the placebo. This robust performance can suzetrigine's ability to manage pain effectively.
One of the most reassuring aspects of suzetrigine is its non-addictive nature. Unlike opioid medications, suzetrigine does not cause nausea, drowsiness, or respiratory depression, which are common issues. The studies found that the most common side effects of suzetrigine include itching, muscle spasms, and rash, but the absence of addiction potential is a significant advantage.
One of the most reassuring aspects of suzetrigine is its non-addictive nature. Unlike opioid medications, suzetrigine does not cause nausea, drowsiness, or respiratory depression, which are common issues. The studies found that the most common side effects of suzetrigine include itching, muscle spasms, and rash, but the absence of addiction potential is a significant advantage.
It's important to note that Suzetrigine should not be taken with certain medications, including erythromycin and the blood pressure/angina medication verapamil, potent inhibitors of CYP3A, a liver enzyme. Food containing grapefruit can also interfere with the medication and should be avoided. This cautionary advice is aimed at ensuring the safety and efficacy of Suzetrigine.
Timing is impeccable for the drug to be approved and in the fight against opiate addiction and deaths. Over a million people have died since the start of this century; there are irreparable costs of billions of dollars in treating people with opioid-related illnesses, addictions, and dependencies. The healthcare system is already struggling to deal with other chronic ailments. I have been at the forefront of stopping opiate prescriptions unless absolutely necessary, and that too for only a few pills at a time. With the new medications in the pipeline and the FDA approval of Suzetrigine, I believe it will be a game changer. I hope the next generation of drugs with reasonable safety profiles will avoid these unnecessary effects plaguing the nation.
There are few instances where these medications are helpful for chronic use and should be under closed supervision of the Pain management physician. More awareness is necessary regarding pain meds, especially opiates and antidotes, which need to be available at every drugstore, and it is unbelievable that the drug works in a few seconds.
It is important to note that there is an antidote to the Opiates overdose, and more awareness is emphasized in the medical communities and general public. I hope the availability of simple drugs like naloxone can save somebody's life.
Naloxone is a medication that rapidly reverses opioid overdoses by blocking the effects of opioids on the brain. It works as an opioid antagonist, meaning it competes with opioids (like heroin, fentanyl, and prescription painkillers) for the same receptors in the brain but does not activate them. This quickly restores normal breathing in people experiencing an overdose.
If anyone is affected by opiate addiction, seek help at SAMHSA or Findreatment.org, which gives various resources for help. Suman Manchireddy MD FACP
Internal Medicine,
Leesburg, VA.
Email : Care@ReliantMD.com
Disclaimer: This is for purely informational and educational purposes only. Seek medical advice before starting any testing or treatment regimen. The data presented here has been extensively researched and condensed for a broader audience, and it should be viewed for educational purposes only. The blogger or blog has no affiliation with any pharmaceutical company.
References:
https://pubmed.ncbi.nlm.nih.gov/33110213/
https://www.nejm.org/doi/full/10.1056/NEJMoa2209870?query=recirc_Semantic#body-ref-r37
https://www.journavx.com/#study-results
https://pubmed.ncbi.nlm.nih.gov/25846613/
https://www.cdc.gov/nchs/products/databriefs/db522.htm
https://bmcemergmed.biomedcentral.com/articles/10.1186/s12873-024-00933-y?utm_source=chatgpt.com#citeas





Thank you for this very informative update on pain management. The opioid crisis is devastating and I am glad to see advances are being made in controlling pain. I know this might sound frivolous, but the main reason I avoid pain relievers is because of how they impact the microbiome.